C. diff infection recurs in up to 35% of cases within 8 weeks after initial C. diff infection diagnosis.1, 2
Recurrent C. diff infection significantly affects hospital quality metrics and reimbursement.
57% of patients with at least one CDI recurrence experienced ≥2 hospital admissions within 12 months.
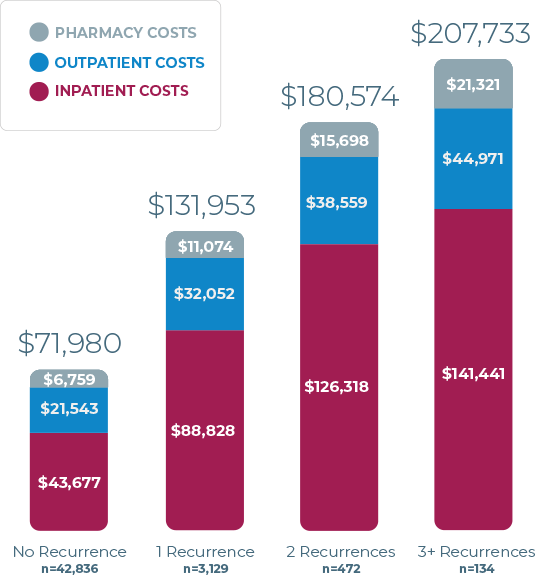
Hospitalizations average 18 days for patients with recurrent CDI. The total, all-cause, and direct medical costs during 12-month period after initial C. diff infection can range from $131K to $207K.3,4

Total, all-cause, direct medical costs during 12-month period after initial C. diff infection.4
Feuerstadt P, et al, Healthcare resource utilization and direct medical costs associated with index and recurrent Clostridioides difficile infection: a real-world data analysis. J Med Econ. 2020;(23)6:603-609. Reprinted by permission from Informa UK Limited, trading as Taylor & Francis Ltd.
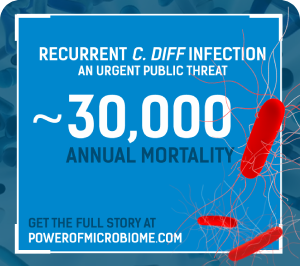
Recurrence accounts for some 75,000 to 175,000 additional cases of C. diff infections per year in the United States.5,6 Furthermore, patients who have had a recurrence are at a higher risk of further C. diff infections.7
After the first recurrence, it has been estimated that up to 60% of patients may develop a subsequent recurrence.3,8-11
In fact, one observational analysis found that upto 85% of patients with recurrent C. diff infection will have a C. diff infection-related readmission within 12 months.12
A systematic literature review found that patients with 3 or more recurrences had a mean of 5.8 inpatient visits per patient in a 12-month follow-up period.4
C. diff infection can be more
dangerous when it recurs.
Can the power of the microbiome help
change the course of treatment?
Share this with colleagues!
References
- Lessa FC, Mu Y, Bamberg WM, et al. Burden of Clostridium difficile infection in the United States. N Engl J Med. 2015;372(9):825-834.
- Cornely OA, Miller MA, Louie TJ, Crook DW, Gorbach SL. Treatment of first recurrence of Clostridium difficile infection: fidaxomicin versus vancomycin. Clin Infect Dis. 2012;55(suppl 2):s154-s161.
- Nelson WW, Scott TA, Boules M, et al. Health care resource utilization and costs of recurrent Clostridioides difficile infection in the elderly: a real-world claims analysis. J Manag Care Spec Pharm. 2021;27(7):828-838.
- Feuerstadt P, Stong L, Dahdal DN, Sacks N, Lang K, Nelson WW. Healthcare resource utilization and direct medical costs associated with index and recurrent Clostridioides difficile infection: a real-world data analysis. J Med Econ. 2020;23(6):603-609.
- Burton HE, Mitchell SA, Watt M. A systematic literature review of economic evaluations of antibiotic treatments for Clostridium difficile infection. Pharmacoeconomics. 2017;35(11):1123-1140.
- Shields K, Araujo-Castillo RV, Theethira TG, Alonso CD, Kelly CP. Recurrent Clostridioides difficile infection: from colonization to cure. Anaerobe. 2015;34:59-73.
- Vincent Y, Manji A, Gregory-Miller K, Lee C. A review of management of Clostridioides difficile infection: primary recurrence. Antibiotics (Basel). 2015;4(4):411-423.
- Leong C, Zelenitsky S. Treatment strategies for recurrent Clostridioides difficile infection. Can J Hosp Pharm. 2013;66(6):361-368.
- Kelly CP. Can we identify patients at high risk of recurrent Clostridium difficile infection? Clin Microbiol Infect. 2012;18(suppl 6):21-27.
- Riddle DJ, Dubberke ER. Clostridium difficile infection in the intensive care unit. Infect Dis Clin North Am. 2009;23(3):727-743.
- Smits WK, Lyras D, Lacy DB, Wilcox MH, Kuiiper EJ. Clostridium difficile infection. Nat Rev Dis Primers. 2016;2(16020):1-47.
- Rodrigues R, Barber GE, Ananthakrishnan AN. A comprehensive study of costs associated with recurrent Clostridioides difficile infection. Infect Control Hosp Epidemiol. 2017;38(2):196-202.